Hidradenitis suppurativa (HS) is a lifelong autoimmune disease that targets sweat glands. It clogs up your glands and can lead to bad infections, scarring, draining wounds. Because of this, HS can be debilitating for anyone who struggles with it.
Essentially, this skin condition causes small, painful acne-like lumps to form under the skin, most commonly in areas where skin rubs against skin, such as the armpits, inner thighs, near the groin, buttocks, or breasts.
For this reason, hidradenitis suppurativa is often mistaken for pimples, boils, or acne cysts. Without proper treatment, these lumps can become more painful, produce a foul-smelling discharge, leak blood or pus, and create scarring. Over time, tunnels known as sinus tracts can form under the skin and can trap bacteria and sweat under the skin, leading to lifelong infection and inflammation.
Hidradenitis Suppurativa (HS) Overview
What is Hidradenitis Suppurativa

Symptoms
Hidradenitis suppurativa often goes misdiagnosed for years. The average time to diagnose HS is 12 years after the first onset of symptoms, which may include:
- Pimples or sores in the armpit
- Underarm cysts or lumps
- Boils, cysts, lumps, or pimples on the thigh
- Sores, cysts, or pimples in the groin area
These pea-sized lumps, pimples, or cysts may persist for weeks or months. They may get larger and eventually break open, leaking pus or blood.

Causes
Hidradenitis suppurativa is more common after the onset of puberty. While the exact cause is unknown, the lumps form when hair follicles become blocked. Experts believe that there could be a connection between HS and:
- Hormones
- Genetic predisposition
- Cigarette smoking
- Excess weight
Risk Factors
While anyone can develop HS, research has shown that those with certain traits are disproportionately affected. These traits and factors that can increase your chance of developing hidradenitis suppurativa include:
- Age: occurrence is higher for those in their 20’s and 30’s
- Sex: females are more likely to develop HS than men
- Race: research shows individuals of color, particularly African American and Hispanic populations, are particularly affected.
- Health Conditions: such as obesity, severe acne, arthritis, diabetes, metabolic syndrome, and inflammatory bowel disease.
- Smoking is also a strong risk factor
Diagnosing
Hidradenitis suppurativa is often misdiagnosed as ingrown hair, acne, or other skin conditions. A hidradenitis suppurativa specialist with experience diagnosing and treating HS will typically look for these three clinical features:
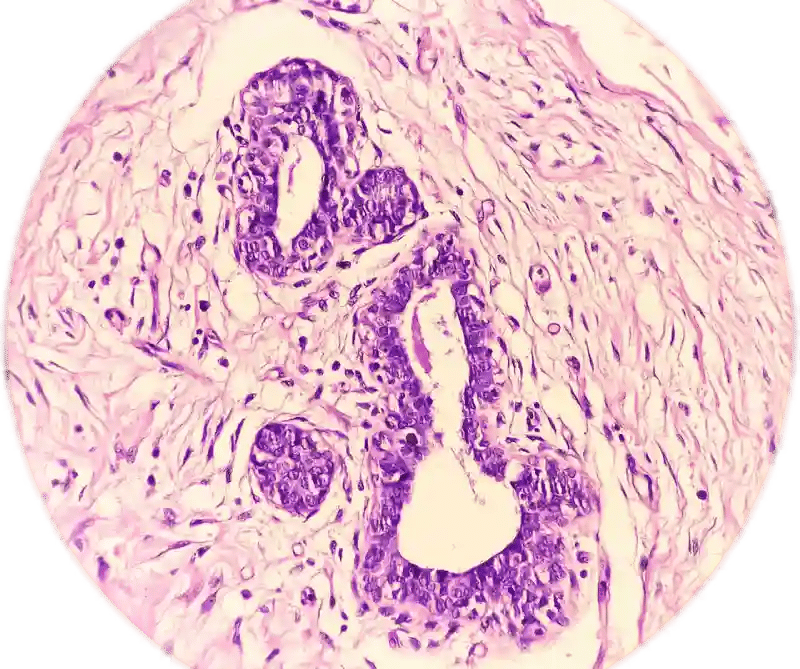
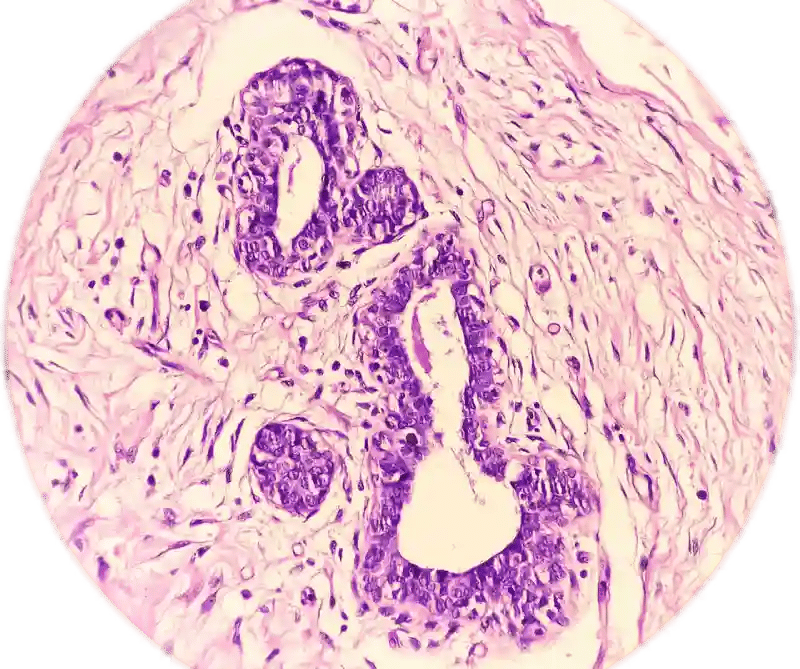
- Typical lesions: abscesses, nodules (abnormal skin growths), scarring, and sinus tracts
- Typical locations: armpits, groin, breast folds, inner thighs, and other areas where skin rubs against skin
- Relapses: occur two or more times in six months
Hidradenitis Suppurativa Treatment
Treating hidradenitis suppurativa occurs in stages, and the approach can vary depending on its progression and severity. When conservative, non-surgical treatments, such as lifestyle changes, topical agents, or immunosuppressive treatments, have failed, HS may need to be treated with surgery.
The surgical treatment, or Stage 3, for hidradenitis suppurativa, typically involves excision of affected tissue and sweat glands. To do this, the surgeon will mark the areas of involvement, including active lesions, sinus tracts, and surrounding scarred skin. Under general anesthesia, wide excision removes all diseased tissue down to healthy subcutaneous fat or fascia.
Depending on the size and location, the wound is left open to heal or closed using various reconstruction techniques. In severe cases, surgeons may need to make extensive excisions, potentially removing entire anatomical regions.
After surgery, patients need careful wound care and follow-up to monitor healing and prevent recurrence. While surgery can provide significant relief, it's important to note that hidradenitis suppurativa may recur, and ongoing medical management is often necessary.
Recovering from hidradenitis suppurativa surgery can take some time, as the procedure often involves the removal of a large area of skin. It can take 4 to 6 weeks—and up to 6 months—for the skin to completely heal. For the first few weeks post-surgery, changing your dressings may be painful, and you may want to ask a family member or friend to assist. Your wounds may also be foul-smelling, and the area may be painful as it heals.
Sometimes, multiple surgeries may be part of your overall hidradenitis suppurativa treatment plan. Your hidradenitis suppurativa specialist may also recommend a combination of continued treatment modalities, including surgery, medications, and lifestyle changes.
Our Doctors
Patient Stories
Find a Hidradenitis Suppurativa Specialist Near Me
Insurance Information
The Institute for Advanced Reconstruction participates in a wide range of insurance plans, including those listed below. However, each physician has their own accepted insurance and hospital affiliations. Before scheduling an appointment, please contact your insurance carrier to confirm that your provider is in-network.
If we are not an in-network provider, our friendly insurance specialists will help you find the most coverage available for your treatment.
- Horizon Blue Cross Blue Shield of New Jersey
- Medicare
- Railroad Medicare
- Aetna
- Cigna
- United Healthcare
- Oxford (Freedom, Liberty)
- MagnaCare
Patient Success Stories
If you suffer from the pain and discomfort of hidradenitis suppurativa, you’re not alone. Explore our patient success stories and discover how surgical hidradenitis suppurativa treatments have improved the quality of life for others like you.
Do you qualify for advanced hidradenitis suppurativa treatment?
If you have progressed to HS Stage 2 or 3, you may be eligible for long-term relief with hidradenitis suppurativa surgery. Contact us today to schedule a consultation with an HS specialist to find out.







