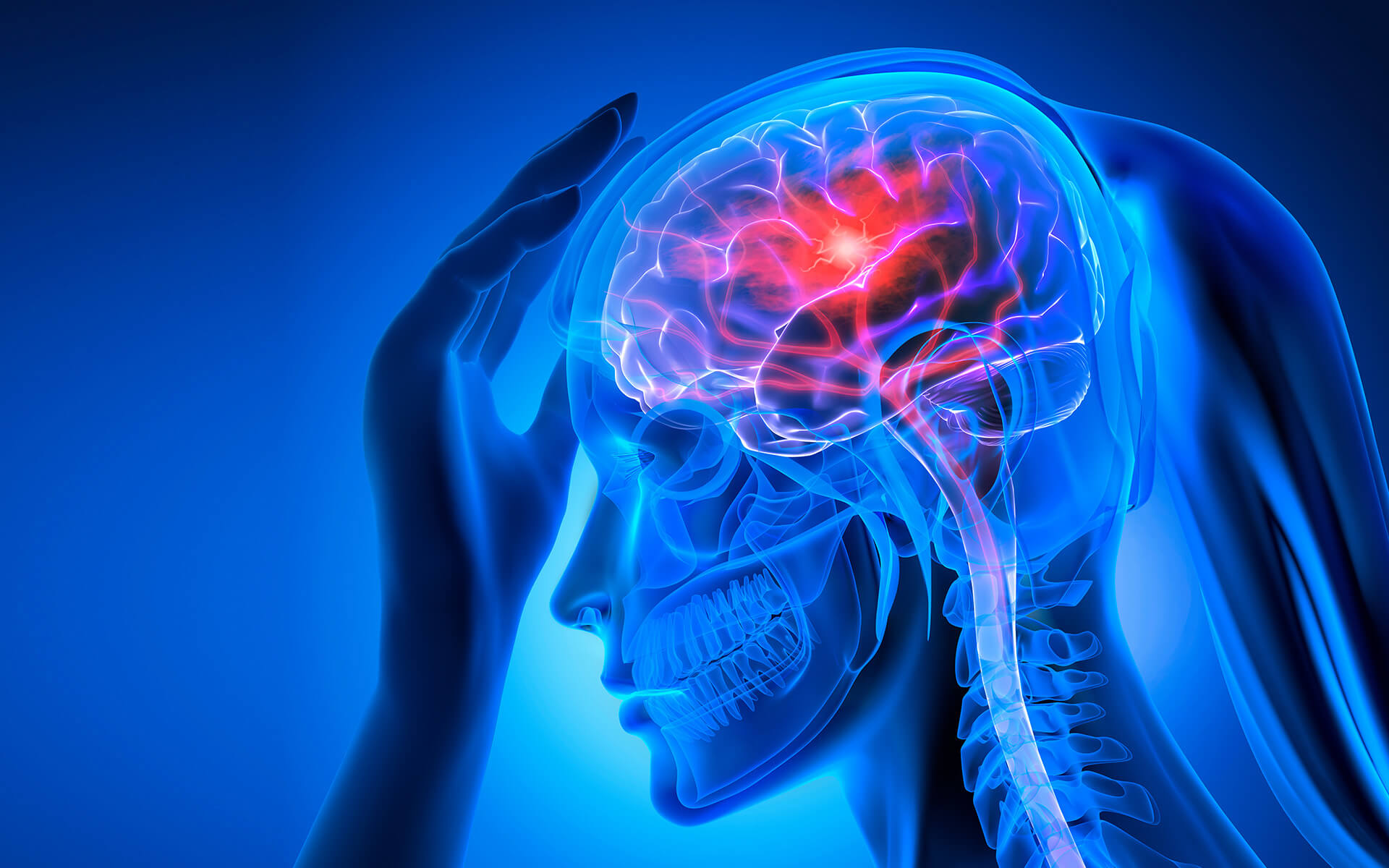
A stroke occurs when the blood flow to an area of the brain is blocked and is considered a true medical emergency. This can be due to a blockage in a blood vessel (called an ischemic stroke) or to bleeding in the brain (called a hemorrhagic stroke). When an area of the brain is without blood flow, it cannot receive oxygen and nutrients. As a result, brain cells quickly begin to die. With early post-stroke treatment, brain damage, disability, and death can be prevented.
Understanding Post-Stroke Treatment Options
Understanding Stroke Recovery & Post Stroke Treatment
Symptoms
If you experience sudden confusion, difficulty walking, difficulty seeing, or a severe headache with no known cause, seek immediate medical attention. During a TIA, stroke symptoms will last between one to five minutes; however, these symptoms should not be ignored just because they are brief. The main symptoms of any type of stroke can be identified and addressed quickly using the acronym FAST:
- Face: Does one side of the face droop when smiling?
- Arms: When you raise both arms, does one drift down?
- Speech: Is speech slurred or troublesome?
- Time: Any of these symptoms warrants a call to 911. The quicker a stroke is treated, the less damage to the brain.
Cause
There are three different kinds of stroke.
- An ischemic stroke is caused by a blood clot in a blood vessel that feeds an area of the brain.
- A hemorrhagic stroke is caused when a blood vessel in the brain bursts.
- A transient ischemic attack (TIA), also known as a “mini-stroke,” occurs when a blood clot briefly blocks a blood vessel, causing temporary disruption of oxygen and nutrients to the brain.
Risk Factors
Certain lifestyle activities or conditions can increase your risk of a stroke, including:
- Smoking
- Diabetes
- High blood pressure
- Heart disease
- Being overweight
- Certain medications like blood thinners or hormones
- Age
Diagnosing Stroke
When a suspected stroke patient arrives at the hospital, a team of experts will get to work immediately to determine what type of stroke occurred. Diagnosing the type of stroke is vital to selecting a treatment approach. To determine this, you’ll likely undergo a few tests, including a physical examination and complete medical history, as well as imaging tests, such as:
- CT scan: This test uses X-ray to create detailed images of the brain and can show if there is bleeding or a blockage in a blood vessel.
- MRI: This test uses magnetic fields and radio waves to create detailed images of the brain and can show more subtle changes in brain tissue compared to a CT scan.
- Angiogram: This test uses X-ray and a special dye to create detailed images of the blood vessels in the brain and show if there is a blockage or a narrowing of a blood vessel.
Post-Stroke Treatment
If you or someone you care about suffers a stroke, healthcare experts will address the condition in two phases.
Emergency Treatment
Emergency stroke treatment is for patients experiencing a stroke caused by a blood clot. This treatment typically consists of IV medication or an injection to break up the clot. The drug must be given within the first 4.5 hours of a stroke to be effective. If you have a large clot that is not completely resolved with drugs, doctors may use a catheter and stent to remove the clot, or may perform an emergency endovascular procedure to work directly inside any blocked blood vessel. Medication may also be delivered directly to the brain via an artery in the groin.
Bleed control is the first line of defense for patients experiencing a hemorrhagic stroke (burst blood vessel). You may be given medication to lower the pressure in your brain or you may have surgery to clip or coil the affected blood vessel. Once you’ve received emergency treatment, you’ll be closely monitored until post-stroke treatment can begin.
Post-Stroke Treatment
A stroke can cause numerous health problems, including
- Behavior changes like depression or anxiety or an increase in impulsivity.
- Changes in speech, swallowing and more
- Pain, numbness or changes in sensation in parts of the body.
- Paralysis on the right side of the body, which can impact movement on the left side of the body.
Post-stroke treatment aims to address these issues and can include one or more of the following:
- Rehabilitation: Rehabilitation is an important part of stroke recovery and may involve a combination of physical therapy, occupational therapy, and speech therapy. These therapies can help a person regain strength, coordination, and function in the affected areas of the body.
- Medications: Several medications may be used to help a person recover from a stroke, including blood thinners to prevent further blood clots, blood pressure medications to help control blood pressure, and medications to improve blood flow to the brain.
- Lifestyle changes: Making healthy lifestyle changes, such as eating a healthy diet, getting regular exercise, and quitting smoking, can help reduce the risk of having another stroke.
- Supportive care: Supportive care may include assistance with activities of daily living, such as bathing, dressing, and grooming, as well as emotional support and counseling to help a person cope with the physical and emotional challenges of recovery.
In cases where other treatments have been unsuccessful or are not possible, Nerve transplant surgery may be an option.
Nerve Transplantation Surgery
Nerve transplantation is a type of surgical procedure that involves transplanting healthy nerve tissue into an area of the body that has been damaged by a stroke or other injury. The goal of nerve transplantation is to restore function to the affected area by providing a new pathway for nerve signals to travel. This procedure can significantly improve paralysis, difficulties swallowing, and pain, numbness, or changes in sensation in particular parts of the body.
The specific details of the surgery will depend on the type of nerve transplantation being performed and the specific area of the body that is being treated. Typically, the patient is placed under general anesthesia. The surgeon will make an incision in the skin to access the affected area and will carefully prepare the area where the nerve transplant will be placed. This may involve removing damaged tissue or preparing a path for the new nerve tissue to follow. Next, the surgeon will transplant the healthy nerve tissue into the prepared area. This may involve attaching the new nerve tissue to the existing nerve endings or using a nerve graft to bridge a gap in the damaged nerve. Lastly, the surgeon will close the incision with sutures or staples and cover it with a dressing.
It will take several months for the new nerve fibers to reach the muscles or skin that were affected and restore movement, function, or sensation. Your physician will likely prescribe physical or occupational therapies to help you regain movement.
Our Doctors
Patient Stories
Find a location
Insurance Information
The Institute for Advanced Reconstruction participates in a wide range of insurance plans, including those listed below. However, each physician has their own accepted insurance and hospital affiliations. Before scheduling an appointment, please contact your insurance carrier to confirm that your provider is in-network.
If we are not an in-network provider, our friendly insurance specialists will help you find the most coverage available for your treatment.
- Horizon Blue Cross Blue Shield of New Jersey
- Medicare
- Railroad Medicare
- Aetna
- Cigna
- United Healthcare
- Oxford (Freedom, Liberty)
- MagnaCare
Related Articles
Patient Resources
Learn more about what to expect when it comes to surgical procedures and treatments at the Institute for Advanced Reconstruction by visiting our patient resource page.
Am I a candidate for nerve transplant surgery?
Your healthcare team will work with you to decide if you’re a candidate for a nerve procedure. Basic qualifications for treatment depend on your age, the severity of your stroke and your ability to participate in therapies once the procedure is complete. Schedule an appointment today to learn more about your options.
