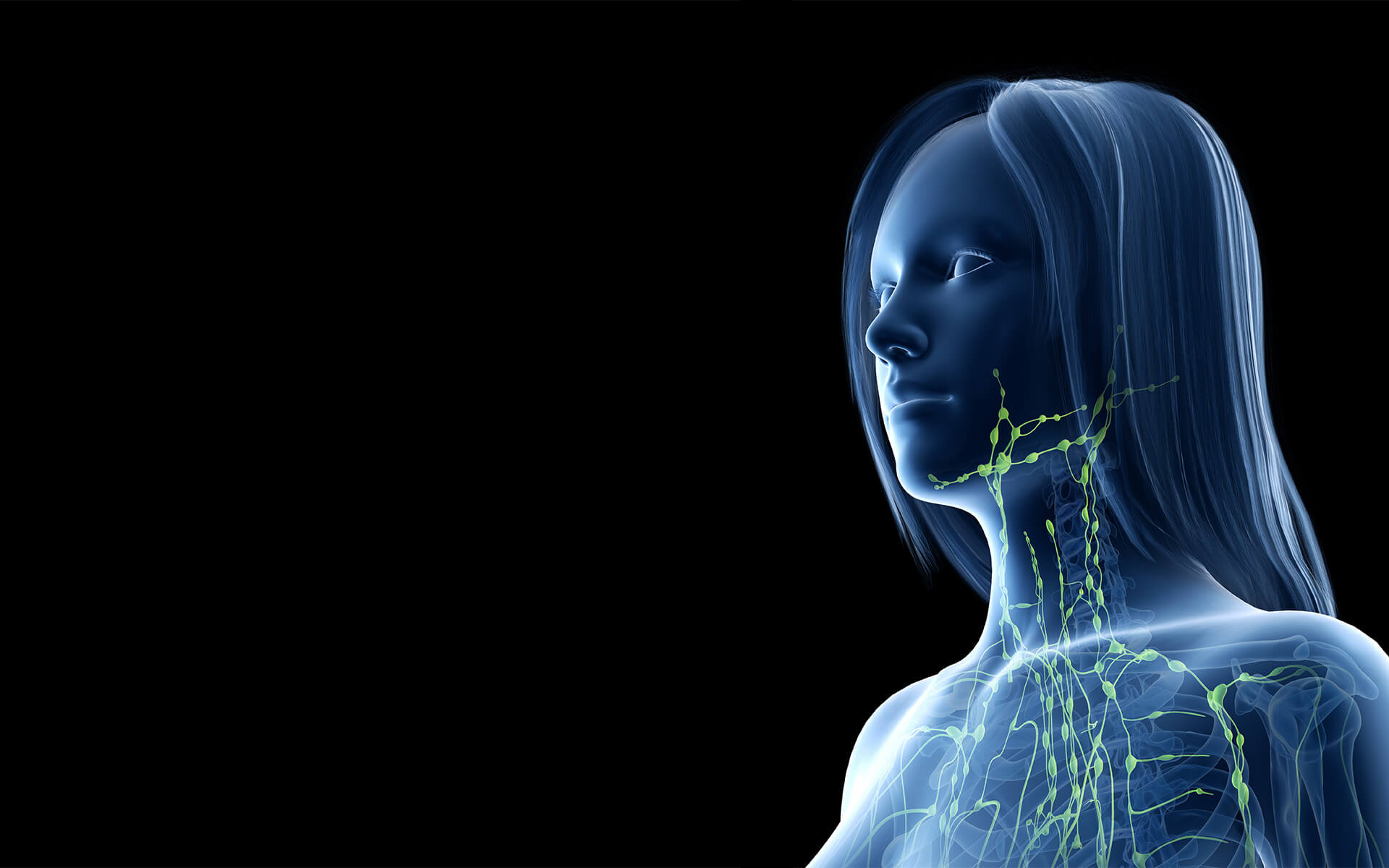
Lymphedema is a chronic condition that often manifests as an abnormal buildup of fluid, causing swelling – most commonly in the arms or legs. This swelling may be present since birth or may develop without a known reason. Lymphedema can also occur after radiation or certain cancer-related surgeries. Initially reversible, lymphedema typically progresses to irreversible, restricting your range of motion and limiting everyday activities.
For many years, the only lymphedema treatment options available were decompressive massage, wraps, and compression. Fortunately, cutting-edge surgical interventions are now available and can provide patients with significant relief. Led by Dr. Joseph Dayan, Director of The Institute for Lymphatic Surgery and Innovation, our center delivers new hope for patients who previously thought they were out of options.
The Institute for Lymphatic Surgery and Innovation
Overview
.webp?width=800&height=533&name=DayanTeam%20(1).webp)
Diagnosis and Prevention
Lymphedema is characterized by significant swelling of part or all of the arm or leg, including fingers and toes. If left untreated, this swelling can progress, restricting your range of motion and impairing your ability to perform everyday activities. A thorough diagnosis can help pinpoint the type of lymphedema a patient has and the cause of the condition.
Signs and Symptoms of Lymphedema
- Swelling of an arm or leg, which may include fingers and toes
- A full or heavy feeling in an arm or leg
- A tight feeling in the skin
- Trouble moving a joint in the arm or leg
- Thickening of the skin, with or without skin changes such as blisters or warts
- A feeling of tightness when wearing clothing, shoes, bracelets, watches, or rings
- Itching of the legs or toes
- A burning feeling in the legs
- Trouble sleeping
- Loss of hair
How is Lymphedema Diagnosed?
Primary lymphedema is congenital and has no direct cause other than a hereditary genetic mutation that leads to a malfunction of the lymphatic system. Secondary lymphedema most often results from injury or obstruction of the lymphatic system, including cancer, cancer treatments, obesity, infection, and trauma. Imaging tests may be used to diagnose cases of lymphedema that are not immediately obvious. These tests may include:- MRI scans use magnetic fields and radio waves to produce a 3D, high-resolution image.
- CT scans use X-ray technology to produce detailed, cross-sectional images and reveal blockages in the lymphatic system.
- Ultrasound tests use sound waves to produce images and help find obstructions within the lymphatic system.
- Lymphoscintigraphy tests use a radioactive dye which is injected and then scanned by a machine to reveal images of the dye moving through the lymph vessels.
Minimizing Your Risk of Lymphedema
If you are at risk for this condition—especially following cancer treatment or surgery affecting the lymph nodes—there are steps you can take to help minimize the likelihood of developing lymphedema:
- Maintain a Healthy Weight: Obesity is a significant risk factor for lymphedema, as excess fat can put pressure on the lymphatic system and impair fluid drainage. Healthy weight management through diet and exercise may reduce your risk.
- Practice Gentle Skin Care: Cuts, burns, and infections can increase inflammation and trigger lymphedema. Keep your skin clean and moisturized, and promptly treat any wounds to prevent complications.
- Stay Active with Low-Impact Exercise: Regular movement helps encourage lymphatic flow. Gentle activities like walking, swimming, and stretching can reduce fluid buildup and support circulation.
- Avoid Excessive Pressure on At-Risk Limbs: Tight clothing, heavy lifting, or repetitive strain on an affected limb may increase swelling. Be mindful of posture and avoid unnecessary pressure on areas vulnerable to lymphedema.
- Follow Post-Surgical Guidelines: If you have undergone lymph node removal or radiation therapy, follow your physician’s recommendations for lymphedema prevention, which may include wearing compression garments, elevating the affected limb, or attending physical therapy.
- Monitor for Early Signs: If you notice persistent swelling, heaviness, or tightness in a limb, consult a specialist. Early intervention can help manage symptoms before they progress.
While not all cases of lymphedema can be prevented, proactive measures can help reduce risk and improve long-term lymphatic health. If you have concerns about lymphedema, The Institute offers expert guidance and treatment options tailored to your needs.
Lymphedema Treatments
There is no cure for lymphedema. Creating a treatment plan for lymphedema is a highly individualized process that focuses on reducing the swelling and preventing complications.
Led by Dr. Joseph Dayan, The Institute for Lymphatic Surgery and Innovation is recognized as a Lymphatic Disease Surgery Center of Excellence (COE) by the Lymphatic Education and Research Network (LE&RN). Our advanced procedures for lymphedema have helped dramatically improve the lives of many of our patients. We specialize in the following lymphedema treatments:
Non-Invasive Treatments
Medication & Therapy
Often, patients are prescribed antibiotics to treat skin infections. Therapy may also be recommended. Complete decongestive therapy (CDT) is a non-surgical treatment plan that includes multiple techniques, incorporating lymphatic draining, compression bandages, certain exercises, and skin care to reduce swelling.
Surgical Procedures for Lymphedema
The surgical team at The Institute for Lymphatic Surgery and Innovation treats both primary and secondary lymphedema with advanced procedures, including:
Lymphaticovenous Anastomosis
Lymphaticovenous anastomosis (LVA) is an advanced microsurgical procedure that creates alternate routes for excess lymphatic fluid to move out of the affected limb. LVA is a minimally invasive procedure that connects the lymphatic vessels to veins in the affected area using a microscope and microsurgical tools. Because it is minimally invasive, LVA surgery can be done either outpatient or over a one-night inpatient stay.
The side effects of LVA typically include bruising, skin staining, and possible infection. Recovery for this type of minimally invasive procedure is faster than more invasive types of surgeries, and patients typically experience a decrease in swelling, increased comfort, and decreased need for compression garments after recovery.
Free Lymph Node Transfer
Free lymph node transfer is a surgical procedure where lymph nodes are harvested from one area of the body and transferred to the areas where lymph nodes have been damaged or removed to improve drainage. This procedure “borrows” lymph nodes from an unaffected area of the body and transplants them along with a blood supply to the affected area using microsurgical techniques. Lymph node transfer surgery is typically in-patient and may require a 1- to 3-day stay.
The risks and side effects of a lymph node transfer are rare but may include vascular compromise that leads to tissues losing their viability or donor-site-associated lymphedema. Recovery time can take 4 to 6 weeks. Expect to work with an occupational or physical therapist in order to get back to your lymphedema therapy quickly to keep swelling down. Some patients will improve quickly (within a matter of weeks), while others may take a few months to a full year to recover. Results can include a reduction or elimination of compression garments, limb volume, and pain/ discomfort, and improvements in limb suppleness and quality of life.
Lymphedema Liposuction
Lymphedema liposuction is a minimally invasive technique used to remove excess fat and scar tissue. Lymphedema liposuction is often performed in combination with lymphaticovenous anastomosis (LVA) or lymph node transfer procedures. Liposuction for lymphedema works by removing excess fat caused by lymphedema in an affected area (when lymphatic fluid spills into surrounding tissues, it can stimulate the growth of fat stem cells).
Liposuction is an outpatient procedure with side effects, including bruising, swelling, redness, or discomfort. If your liposuction is combined with another lymphedema surgical procedure, it may become an inpatient stay. The recovery time for liposuction is typically around 4 to 6 weeks, after which point the surgical swelling should go down, and you should be able to see visible results of a reduction in mass from the affected area.
Lymphedema Mass Excision
If lymphedema has resulted in a mass hanging from the inside or outside of a patient’s thigh, a lymphedema mass excision procedure can be done to surgically remove the mass and make walking and movement of the leg easier. This type of procedure is a more radical debulking procedure compared to liposuction, involving the removal of damaged skin and fat from the affected area down to the muscle and a skin graft to transplant skin from an unaffected area. Lymphedema mass excision is typically performed on patients with advanced lymphedema.
The risks of a mass excision procedure are higher than those of liposuction and can include bleeding (hematoma), necrosis of the grafted skin, infection, delayed wound healing, blood clots, scarring, and a recurrence of lymphedema. This intensive inpatient procedure typically requires a hospital stay, with an in-hospital recovery period of weeks to months. Some patients may require blood transfusions or additional surgeries.
Breast Reconstruction with Lymphedema Surgery
For lymphedema patients who have had a mastectomy, breast reconstruction can be performed at the same time as one of the above-mentioned lymphedema surgical procedures. Breast reconstruction uses a woman's own tissues or an implant to recreate a breast lost to a mastectomy.
Breast reconstruction surgery can have side effects, including bleeding (hematoma), blood clots, fluid buildup, delayed wound healing, tissue necrosis, infection, and problems with a breast implant (leaking, rupture, or rippling.) Recovery from breast reconstruction surgery can take anywhere from 8 weeks to a year. Your total procedure and recovery time will depend on what other lymphedema procedures are being performed concurrently. Your surgeon can help you understand what to expect with a combination procedure such as lymphedema surgery and breast reconstruction.
Lymphedema Webinars

Modern Concepts in Surgical Treatment and Prevention of Lymphedema
View Dr. Dayan's webinar on Modern Concepts in Surgical Treatment and Prevention of Lymphedema for expert insights into the latest advancements in managing and preventing this condition.
Lymphedema Podcasts

Dr. Dayan Discusses Lymphedema on Wellness Unmasked Podcast
In this episode of Wellness Unmasked, Dr. Joseph Dayan brings clarity and hope to breast cancer survivors living with lymphedema.
Meet the Surgeons
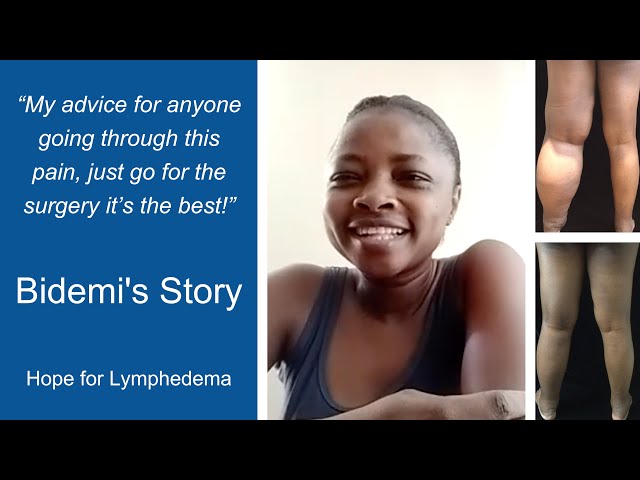
Patient Stories
Eligibility for Lymphedema Treatment
Patients must have a diagnosis of Lymphedema before visiting The Institute for Advanced Reconstruction. To qualify for treatment, patients must also:
- Have a BMI of 50 or less
- Have 3-6 months of manual lymphatic drainage
Educational Resources
News & Highlights
Dr. Dayan Patient Featured on The Current with Matt Galloway
Dr. Joseph Dayan Featured in the Daily Mail for Groundbreaking Lymphedema Research
Institute for Advanced Reconstruction Announces First-of-Its-Kind Prospective Study of GLP-1 Receptor Agonists for Lymphedema Treatment
Weight Loss Drugs Show Promise in Treating Breast Cancer-Related Lymphedema
Lymphedema Specialist Near Me

Recent Publications
Manuscripts & Abstracts
- Brown S, Kokosis G, Graziano FD, Haran O, Smith-Montes E, Zivanovic O, Ariyan CE, Coit DG, Coriddi M, Mehrara BJ, Dayan JH. Immediate Lymphatic Reconstruction with Vascularized Omentum Lymph Node Transplant: Reducing the Risk of Both Painful Contracture and Lymphedema. Plast Reconstr Surg Glob Open. 2024
- Ashinoff RL, Chang EI. Lower extremity lymphedema. In: Collins KA, Eidt JF, Mills JL, Butler CE, eds. UpToDate. Waltham, MA; 2019.
Coordinating Insurance and Billing
It is always advisable to discuss anticipated tests and procedures with your doctor prior to an appointment. We also recommend checking with your insurance provider to make sure all services and procedures are covered by your plan.
Additionally, some health insurance policies require that you obtain a referral from your primary care provider before seeing a specialist. If this is the case, our friendly patient intake team will work with your physician to obtain authorization from your insurance carrier.
Patient Referrals
The Institute respects the relationship you have with your patients. When you refer a patient to us, we act as an extension of your care and recognize that the patient still looks to you as their primary doctor.
Our care team is sensitive to the pain and discomfort that many patients with lymphedema experience. We promise to work as efficiently as possible to determine the best course of treatment for your patient. Referring physicians can expect open communication, transparency, and prompt follow-up, including visit summaries, test results, surgery summaries, and discharge notes.

.webp)