Genetic counseling helps individuals and families understand their risk for hereditary cancers by reviewing medical histories, explaining genetic testing, and offering guidance on managing risks. By providing expert insights and personalized support, we help you make informed decisions and navigate your cancer prevention journey with confidence.

What is Genetic Counseling?
Genetic counseling for cancer is a specialized service that provides information, guidance, and support to individuals and families who may be at an increased risk of developing certain types of cancers due to inherited genetic mutations. The primary goals of genetic counseling are to:
- Assess an individual's personal and family medical history to determine their risk of carrying a hereditary cancer syndrome or genetic predisposition.
- Explain the implications of genetic testing and help individuals make informed decisions about whether to undergo genetic testing for specific cancer-related genes.
- Interpret the results of genetic tests and provide guidance on the associated cancer risks, screening recommendations, and preventive options.
- Facilitate informed decision-making about potential risk-reducing strategies, such as increased surveillance, prophylactic surgery, preventative medication, or lifestyle modifications.
- Provide emotional support and resources for coping with the psychological impact of being at high risk for cancer or carrying a genetic mutation.
- Discuss the risks and implications for family members and provide guidance on sharing genetic information with relatives.
Genetic counselors are healthcare professionals with specialized training in medical genetics and counseling. They work closely with other medical specialists, such as oncologists, surgeons, and psychologists, to provide comprehensive care and support for individuals and families affected by hereditary cancer syndromes. Genetic counseling plays a crucial role in promoting awareness, facilitating informed decision-making, and empowering individuals to take proactive steps in managing their cancer risk. People who undergo genetic testing for cancer may consult a genetic counselor for insight into the implications of their test results and create a plan of action for treatment.
Understanding Genetic Testing
Multi-Panel Genetic Testing
About 1 in 6 people in the United States have a gene mutation that puts them at higher risk for developing cancer. Multi-panel genetic testing analyzes your DNA to check for mutations in several genes associated with various types of cancers, including BRCA 1, BRCA 2, TM, p53, CHEK2, PTEN, and CDH1. People get tested to determine their risk of developing cancers such as breast, ovarian, colorectal, and prostate cancers. Individuals with close relatives diagnosed with these cancers at an early age or multiple affected relatives may consider getting a multi-panel genetic test. A positive test means you have an increased lifetime risk for certain cancers, and early, more frequent screening is recommended. A negative test result indicates an average risk of those cancers, and standard screening guidelines should be followed.
BRCA Genetic Testing
The BRCA1 and BRCA2 genes are both tumor suppressor genes that can cause cancer if a mutation occurs. When working properly, they help repair damaged DNA, ensuring the stability of each cell's genetic material. We all have two copies of each of these genes. Mutations in one or both copies of these genes lead to faulty protein production, which increases lifetime cancer risks.
While mutations in either gene raise cancer risks, there are some key differences. BRCA1 mutations most notably increase the risk of breast and ovarian cancers. A BRCA1 mutation carrier has a 55-65% lifetime risk of breast cancer and a 39% risk of ovarian cancer. BRCA2 mutations also raise breast cancer risk, though not as much as BRCA1. The lifetime risk of breast cancer with a BRCA2 mutation is about 45%. However, BRCA2 has a stronger association with other cancer types. It increases ovarian cancer risk to about 17%, as well as the risk for melanoma, pancreatic, stomach, gallbladder, bile duct, and prostate cancers in both men and women. So, while both genes significantly affect cancer risks when mutated, BRCA1 has a bigger impact on female reproductive cancers, while BRCA2 has a broader spectrum of associated cancers.
Common Genetic Mutations
The TP53 gene, also known as the p53 gene, plays a crucial role in suppressing tumor growth by regulating cell division and triggering apoptosis (programmed cell death) in damaged cells. Mutations in the TP53 gene can lead to uncontrolled cell growth and the development of various cancers, including breast, ovarian, colorectal, and lung cancers. TP53 mutations are relatively common, found in approximately 50% of all human cancers.
The CHEK2 gene is involved in DNA repair and cell cycle regulation. Mutations in this gene can impair the body's ability to repair damaged DNA, increasing the risk of cancers such as breast, colorectal, and prostate cancers. CHEK2 mutations are relatively rare, occurring in approximately 1-2% of the population.
The PTEN gene is a tumor suppressor gene that regulates cell growth, proliferation, and migration. Mutations in the PTEN gene can lead to increased cell growth and survival, contributing to the development of cancers such as breast, thyroid, endometrial, and prostate cancers. PTEN mutations are found in a significant proportion of these cancers, ranging from 5% to 30%, depending on the cancer type.
The CDH1 gene plays a crucial role in cell adhesion and maintaining the structure of epithelial tissues. Mutations in this gene can disrupt cell-cell adhesion, leading to increased cell mobility and invasion, which are hallmarks of cancer metastasis. CDH1 mutations are associated with an increased risk of developing gastric cancer and lobular breast cancer. However, CDH1 mutations are relatively rare, occurring in less than 1% of the population.
For patients with mutations in these genes, the implications can vary depending on the specific gene and the type of mutation. In general, individuals with mutations in these genes have an increased lifetime risk of developing certain cancers. Early and frequent cancer screening, risk-reducing measures (such as prophylactic surgery or medications), and lifestyle modifications may be recommended to help manage the elevated cancer risk. Genetic counseling is also important to understand the implications of the specific mutation and develop an appropriate screening and management plan.
When to See a Genetic Counselor
Genetic counseling is recommended for anyone with concerns about their personal or family history of cancer to help assess their risk, facilitate informed decision-making, and provide support and resources for managing that risk.
In general, having first-degree relatives (parents, siblings, children) or other blood relatives diagnosed with cancer suggests a possible inherited mutation. The more affected relatives there are, and the earlier the ages of diagnosis, the higher the risk an inherited genetic mutation exists in the family. If your personal or family history includes any genetic mutation-related cancer types, you might want to consider seeing a genetic counselor. It is recommended to seek genetic counseling for cancer risk assessment if you exhibit any of the following characteristics:
Family History of Cancer
If an individual has a close blood relative (parent, sibling, child) with certain cancers, especially those diagnosed at a younger age, it may indicate an inherited genetic predisposition. Genetic counseling can help evaluate the pattern of cancers in the family and determine if genetic testing is appropriate.
Specific Types of Cancers
Some types of cancers, such as breast, ovarian, colorectal, and pancreatic cancers, are more likely to have a hereditary component. Genetic counseling is often recommended for individuals diagnosed with these cancers, especially at a young age or with certain characteristics.
Multiple Cancers
If an individual has been diagnosed with more than one type of cancer, it may suggest an underlying genetic cause. Genetic counseling can help evaluate the potential for hereditary cancer syndromes.
Ethnic Background
Certain ethnic groups, such as Ashkenazi Jewish, have a higher prevalence of specific genetic mutations associated with cancer risk. Genetic counseling can help assess the need for testing based on ethnic background.
Considering Genetic Testing
Before undergoing genetic testing for cancer-related genes, such as BRCA1, BRCA2, or multi-gene panels, it is recommended to have genetic counseling to understand the implications, benefits, and limitations of testing.
Reproductive Planning
Individuals with a known hereditary cancer syndrome or genetic mutation may benefit from genetic counseling when planning to have children to understand the risks of passing on the mutation and options for preimplantation genetic testing.
Family Communication
Genetic counselors can provide guidance on how to communicate genetic information and test results to family members who may also be at risk.
Treatment
If you test positive for a genetic mutation, your physician can help determine which prevention options make the most sense based on your mutation type, cancer family history, lifestyle factors, and risks of each option. Ongoing specialized screenings are also crucial for early cancer detection.
Non-Surgical Treatments
Increased Surveillance
More frequent and intensive cancer screening, such as regular mammograms, breast MRIs, colonoscopies, and other imaging tests, depending on the specific mutation and associated cancer risks.
Preventative Medication
The use of medications like tamoxifen or raloxifene to reduce the risk of breast cancer in high-risk individuals, particularly those with BRCA1/2 mutations.
Risk-Reducing Lifestyle Modifications
Adopting a healthy diet, regular exercise, maintaining a healthy weight, and avoiding smoking may help reduce cancer risk.
Surgical Treatments
Prophylactic Mastectomy
Removal of one or both breasts to reduce the risk of breast cancer, particularly for BRCA1/2 and TP53 mutation carriers.
Prophylactic Salpingo-Oophorectomy
Removal of the ovaries and fallopian tubes to reduce the risk of ovarian and fallopian tube cancers is often recommended for BRCA1/2 mutation carriers. A referral to a GYN oncologist is warranted at that time.
Prophylactic Hysterectomy
Removal of the uterus, which may be recommended for some CDH1 mutation carriers to reduce the risk of endometrial cancer. A referral to a GYN oncologist is warranted at that time.
Lumpectomy
Surgical removal of cancerous tissue from the breast while preserving the surrounding healthy tissue. This procedure is often recommended for early-stage breast cancer and may be followed by radiation therapy to minimize the risk of recurrence. A thorough discussion with a surgical oncologist is essential to determine the best approach based on individual circumstances.
Our Genetic Testing/Counseling Services
The Breast Center of New Jersey offers genetic testing services for high-risk patients through partner providers. Having access to these critical services can help identify inherited gene mutations that may increase your risk of certain cancers, allowing for more personalized screening plans and preventive measures. By understanding your genetic profile, you and your healthcare team can make more informed decisions about your care, potentially catching cancer earlier or even preventing it altogether.
We also partner with ReVital Cancer Rehabilitation, a comprehensive program designed to enhance the quality of life for cancer patients at all stages of their journey. This specialized therapy addresses the common side effects of cancer and its treatment, including pain, fatigue, cognitive issues, and mobility challenges. By focusing on three critical phases - pre-treatment, during treatment, and post-treatment survivorship - ReVital's highly trained therapists develop tailored plans to meet each individual's unique needs and goals. The program aims to help patients regain independence, improve physical and cognitive function, and manage persistent symptoms. With expertise in physical, occupational, and speech therapy, ReVital therapists work to restore overall well-being, enabling patients to return to their daily activities and roles with greater ease and confidence.
Contact Us Today
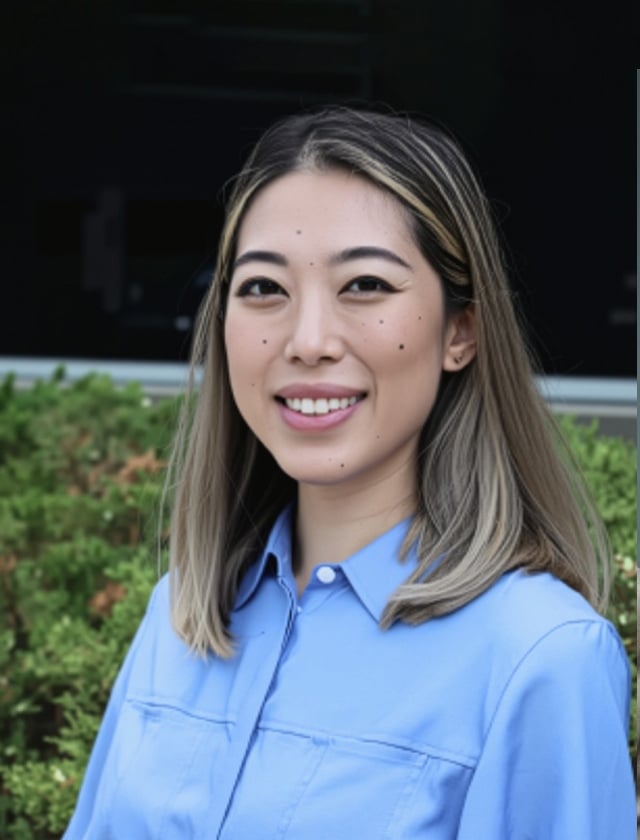
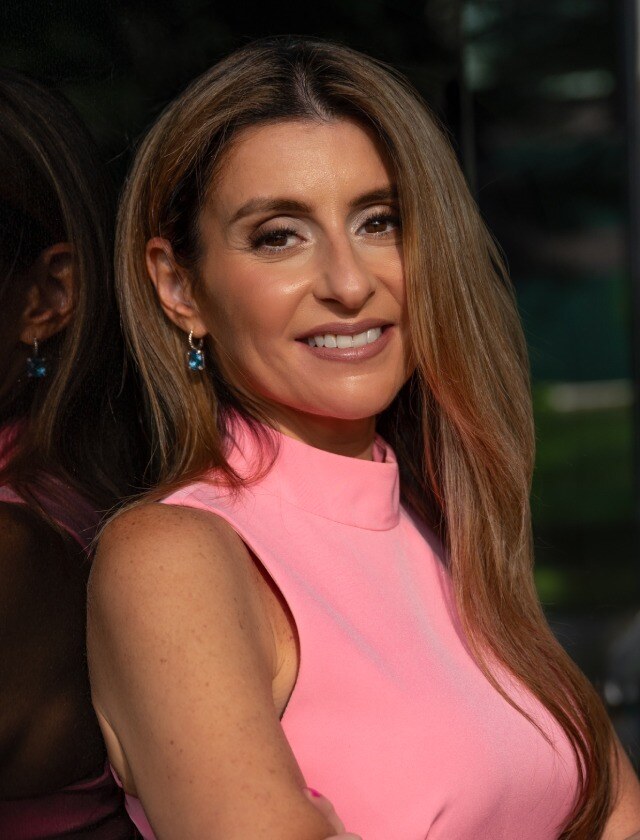
Our Doctors
The providers at The Breast Center of New Jersey, a division of The Institute, are leaders in treating breast cancer. Our team of surgical specialists is experienced with advanced breast cancer removal and reconstruction techniques.

Am I a Candidate For Genetic Testing?
If you have a strong family history of breast, ovarian, or other cancers, make an appointment to discuss genetic testing with our caring team of breast specialists—we help identify personalized risk factors and empower patients with the knowledge to take proactive steps toward vigilant prevention or early detection.

%201.svg)







-min.png)
.webp)






















-1.jpeg)

