A mastectomy is the removal of one or both breasts to treat or prevent breast cancer. It may involve removing nearby lymph nodes and can be followed by reconstruction. At The Breast Center of New Jersey, we provide personalized support to help you through the entire mastectomy process, from decision-making to recovery.
Mastectomy
Conditions Treated
- Ut enim ad minim veniam
- Lorem ipsum dolor sit amet
- Sed do eiusmod tempor incididunt
- Ut enim ad minim veniam
- Lorem ipsum dolor sit amet
- Sed do eiusmod tempor incididunt

What Is a Mastectomy?
A mastectomy is the surgical removal of a breast, typically done to treat or prevent breast cancer. During a mastectomy, the surgeon will remove the entire breast with or without the nipple/areolar complex. Sometimes, lymph nodes or other cancerous tissue near the breast may be removed to prevent cancer spread and stop recurrence. Mastectomies may be recommended for cancer treatment. It can also be a preventive measure for high-risk patients. After a mastectomy, breast reconstruction can be performed to recreate the shape of the removed breast.
Do I Need a Mastectomy?
Mastectomies are performed on those who have been diagnosed with breast cancer or those at high risk of developing breast cancer. The patient may be advised by their physician to undergo a mastectomy if the cancer has spread to multiple areas of the breast or if other treatments like lumpectomy/radiation are not feasible options. Mastectomies may eliminate the cancer and prevent it from recurring or spreading further.
For those with a strong family history of breast cancer or a genetic mutation known to increase breast cancer risk, a preventive mastectomy may be recommended for the patient. Some women elect to have mastectomies as a preventive measure before any sign of cancer. It is a difficult decision; people should discuss their personal risk factors with a physician and learn about the procedure, potential side effects, and recovery to determine if a mastectomy is their best option. All factors are considered, given their medical history and goals.
Types of Mastectomies
When facing breast cancer or evaluating options for cancer prevention, deciding on the type of mastectomy procedure is an important choice. Your medical team will extensively evaluate your condition and then recommend the mastectomy technique that is projected to safely eliminate or prevent occurrence while retaining the most natural shape.

Nipple Sparing Mastectomy
Unlike a total mastectomy, which removes the entire breast, including the nipple and areola, a nipple-sparing mastectomy is a procedure that removes breast tissue but keeps the nipple area intact. This allows for a more natural reconstruction result. During the operation, the surgeon takes out all glandular and fatty breast tissue while preserving nerves, blood vessels, and the nipple. Since any remnants of breast cells could develop into cancer, nipple-sparing mastectomy candidates are carefully selected based on the size and location of the cancer. The procedure carries risks like infection, tissue damage, or lack of sensation after healing.

Prophylactic Mastectomy
A prophylactic mastectomy refers to electively removing one or both healthy breasts to prevent future breast cancer from developing. For those with genetic mutations like BRCA1 or BRCA2 that increase the risk of developing breast cancer, removing tissue that could become cancerous reduces the chances of actually getting breast cancer later on. A prophylactic mastectomy lowers the risk of breast cancer and provides emotional comfort for some patients. Those considering prophylactic mastectomy should discuss genetic testing and reconstruction options with their care team.
What to Expect
Before Your Mastectomy
Before your mastectomy procedure, you will meet with your physician and care team to talk through your specific breast cancer diagnosis or risk profile, treatment options, and surgery plans. Your physician will perform imaging tests on your breasts, like a mammogram, ultrasound, or MRI, to help determine the size and location of any tumors. They may also order blood work or other tests to ensure you are healthy enough for the operation. You will discuss details like whether one or both breasts need removal, if lymph nodes should be tested, and any reconstruction goals with your plastic surgeon. Your exact surgery plan will depend on your unique cancer stage, prognosis, genetics, and goals.
During the Procedure
On the day of mastectomy surgery, you cannot eat or drink anything for at least 6-12 hours before surgery. Once at the hospital, your breasts will be marked and prepped; then, you will receive general anesthesia in the operating room itself. Depending on your specific case, the full mastectomy procedure typically takes anywhere from 2-4 hours. The surgeon carefully removes breast tissue, sometimes along with lymph nodes/pectoralis fascia, if necessary. Often, reconstructive plastic surgeons will begin reshaping the breast area during this same surgery session right after the mastectomy. Techniques like nipple-sparing methods aim to retain a natural look, if possible, based on your diagnosis. Afterward, you wake up in a recovery room for close monitoring before moving to a regular hospital room.
After the Procedure
During the weeks after your mastectomy, you can expect some wound care, surgical drain maintenance, medications to reduce pain and infection risk, and follow-up appointments to closely track your healing progress. Most patients are able to return to their normal routine around 2-6 weeks after surgery. Many find emotional counseling useful for coping with the life adjustment process during this period. Once fully healed after several months, options like breast prosthetics or staged reconstructive surgery can be discussed to achieve your cosmetic goals. Those with a cancer diagnosis will require continued exams to monitor for potential recurrence yearly.
Recovery
The recovery period after a mastectomy surgery typically lasts several weeks. During initial recovery in the hospital and two weeks following discharge, patients can expect moderate levels of post-surgical pain and discomfort from the incision site as the skin and tissues heal. To manage pain, prescription medications are often used immediately after surgery, with a transition to over-the-counter pain relievers over the first couple of weeks. Surgical drains are usually left to prevent fluid buildup and are removed around 1-2 weeks post-op once drainage volume decreases.
Mobility will be limited, so assistance with daily tasks is necessary; light activity like walking may resume shortly after surgery, with more strenuous exercise restricted until authorized by your surgeon. The operated area is extremely tender and will remain numb or tingling for a few months. Some swelling, tightness, or sensations of pulling at the chest and underarm area are common. Many patients experience fatigue, trouble sleeping, and can feel emotional during the adjustment period. While the initial recovery period brings physical limitations and discomfort, symptoms gradually subside over 2-6 weeks, allowing patients to return to regular activity.
Follow-Up Care
Typical follow-up care needed after a mastectomy includes:
- Wound care: The incision site will need regular cleaning/dressing changes to prevent infection while the skin heals. Drainage tubes also need proper maintenance until removed at a post-op visit.
- Symptom monitoring: Physicians will track symptoms like pain, swelling, immobility, numbness, tingling, or fluid buildup to ensure proper healing. Issues like infection, inadequate drainage, or blood clots must be addressed promptly.
- Physical therapy: Many patients undergo PT starting about 2-6 weeks post-surgery to regain strength and range of motion. The therapist helps reduce associated swelling or stiffness at the shoulder/arm on the side of surgery.
- Prosthesis or reconstructive surgery fitting: Around 6-8+ weeks after surgery, once the skin has healed, a breast prosthetic can be fitted or follow up with your surgeon for reconstructive techniques.
- Emotional support: Counseling often helps women cope with the psychological and emotional aspects surrounding body image changes and grief over losing a breast. Support groups also provide assistance.
- Medical oncology follow-ups: Cancer patients need continued surveillance - usually exams and imaging every few months. Further treatments may be warranted if recurrence is detected.
Contact Us Today
Incididunt Ut Labore
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et hyperlink text. Ut enim ad minim veniam. Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam.
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam. Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam.
Nemo enim
Nemo enim ipsam voluptatem quia voluptas sit aspernatur aut odit aut fugit, sed quia consequuntur magni dolores eos qui ratione voluptatem sequi nesciunt. Neque porro quisquam est, qui dolorem ipsum quia dolor sit amet, consectetur, adipisci velit, sed quia non numquam eius modi tempora incidunt ut labore et dolore magnam aliquam quaerat voluptatem.
Lorem ipsum
- Ut enim ad minim veniam
- Lorem ipsum dolor sit amet
- Sed do eiusmod tempor incididunt
- Ut enim ad minim veniam
- Lorem ipsum dolor sit amet
- Sed do eiusmod tempor incididunt
Contact Us Today
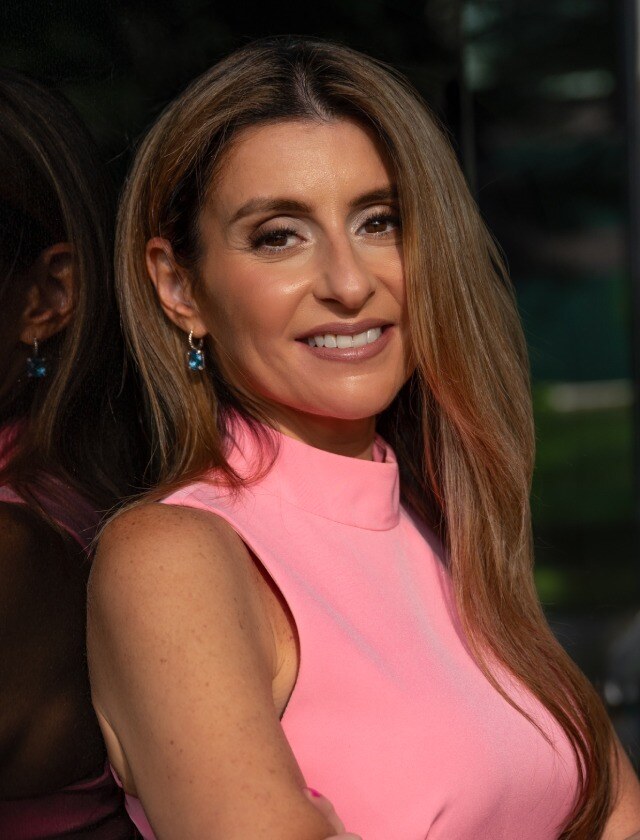
Real people. Real results.
Meet John Doe,
Who underwent Shoulder and Elbow Arthritis For Shoulder.
“Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Quis ipsum suspendisse ultrices gravida. Risus commodo viverra maecenas accumsan.”

Schedule an Appointment
Preparing for a mastectomy can be an emotionally taxing experience. The compassionate team at Breast Center of New Jersey, a division of The Institute, is here to support, guide, and comfort you each step of the way with care and expertise. We encourage you to schedule a consultation at our specialized center to discuss your breast cancer treatment options.

%201.svg)


-1.jpeg)






-min.png)
.webp)






















.jpg?width=439&quality=high)



















