Surgery for Graves’ Disease Solves Woman’s Eye Problems
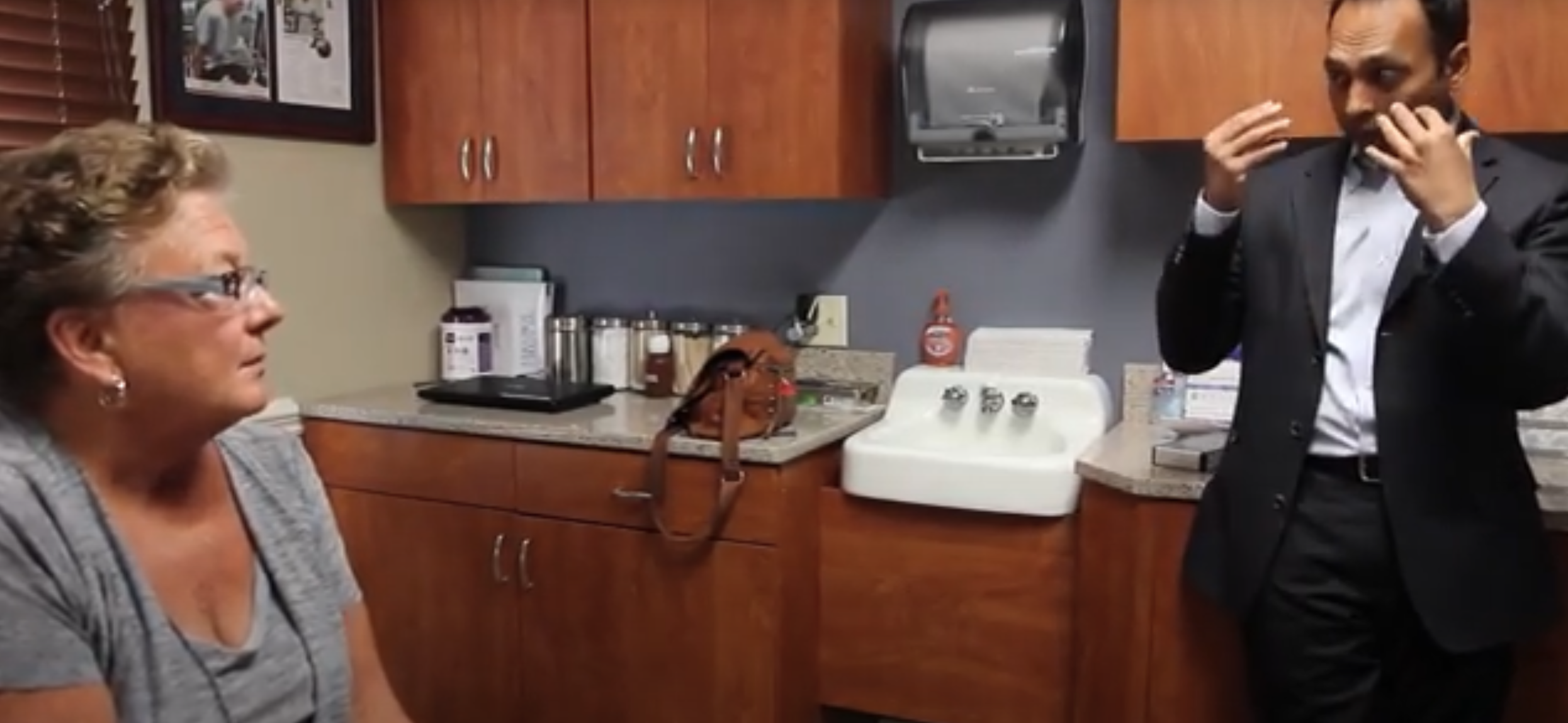
Dr. Tushar Patel Performs Orbital Decompression
Rebecca Smith was biding her time. She needed eye surgery but had to wait two years to do it.

Rebecca Before Orbital Decompression for Graves’ Ophthalmopathy
That’s because the 39-year-old resident of Monmouth County, New Jersey, and mother of two developed Graves’ disease shortly after the birth of her second child. This led to the characteristic eye problems that caused her to experience pressure build-up on the optic nerve, with extensive eye swelling. “It looked like I didn’t sleep at all or that I had severe allergies,” she said.
Although Smith began with oral medication, her doctor explained that following the typical two-year active phase of the disease, corrective surgery would be indicated to relieve the orbital pressure build-up.
While Graves’ disease may develop at any age in both women and men, it more commonly affects women aged 20 years or older. It affects nearly 14 in 100,000 people.
According to the Graves’ Disease and Thyroid Foundation, Graves’ must be treated to avoid complications such as bone/muscle wasting, heart problems, and a very serious, life-threatening event called thyroid storm (when the thyroid gland suddenly releases large amounts of thyroid hormone in a short period of time).
In its more advanced stages, orbital decompression surgery, such as that performed by Dr. Tushar Patel of The Institute for Advanced Reconstruction, becomes necessary to reverse the effects of this condition. The procedure involves removing excess fat from the orbital cavity, as well as expanding the orbital wall to alleviate pressure and congestion in and around the eyes. This will correct issues such as orbital congestion, pain, eye bulging, and eyelid disfigurement.
Smith heard of Dr. Patel through a friend but also read up on him and his patients’ testimonies on his practice website. She underwent surgery on one eye in March 2014 and, as is customary, had the second eye surgery six weeks later. Both surgeries were performed at Jersey Shore University Medical Center.

Rebecca After Orbital Decompression for Graves’ Ophthalmopathy
Smith never considered another doctor after she met Dr. Patel. “I only did a consultation with Dr. Patel since that’s how comfortable I felt with him right from the beginning.” While Dr. Patel extensively explained the surgery to her, he and his staff were also accommodating and kind to Smith’s children, whom she brings to every appointment. That added ‘extra’ was important to her as well as how he explained things to her.
“Some doctors expect you not to understand. Dr. Patel spoke, so I didn’t feel that he was ‘giving me the speech.’ He was there; he was present, talking to me about my situation. Even though he has done this surgery many times, he was not talking to me like I was just the next case.”
Dr. Patel also reassured her about the procedure. “I wasn’t scared. The risks were so low; they were basically the risks of general surgery.”
Smith explained that while the second surgery required some internal sutures that caused a bit of discomfort, the first was so easy that she didn’t even need the pain medication the hospital provided. She had the cell phone numbers of Dr. Patel and his staff and felt comfortable that she could call any of them at any time. She was able to resume her normal life after a brief period of recovery.
Rebecca Smith is three months out from her final surgery with Dr. Patel. She is in remission from Graves’ Disease, but she does see her endocrinologist every six months for a check-up to make sure it does not return.