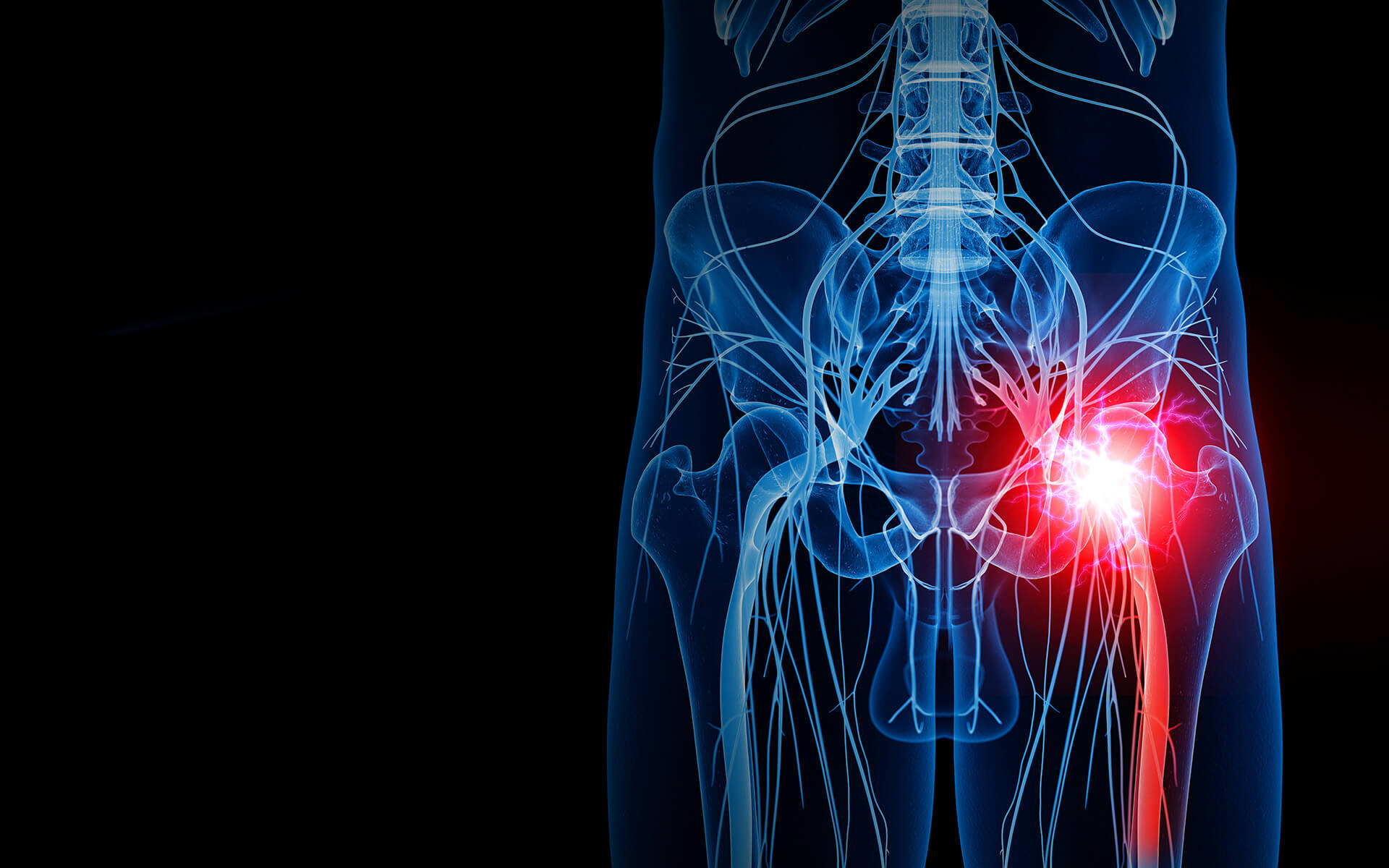
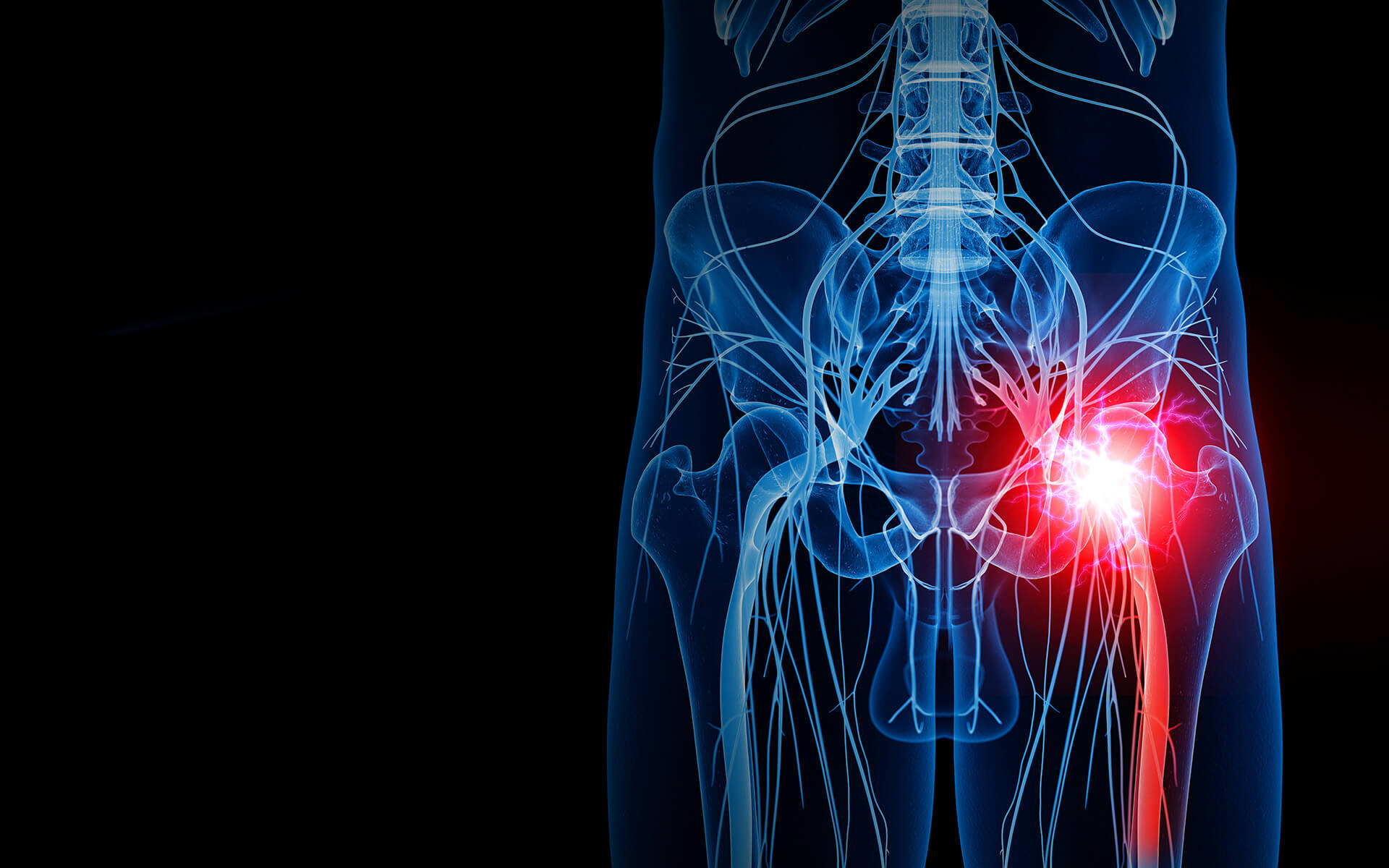
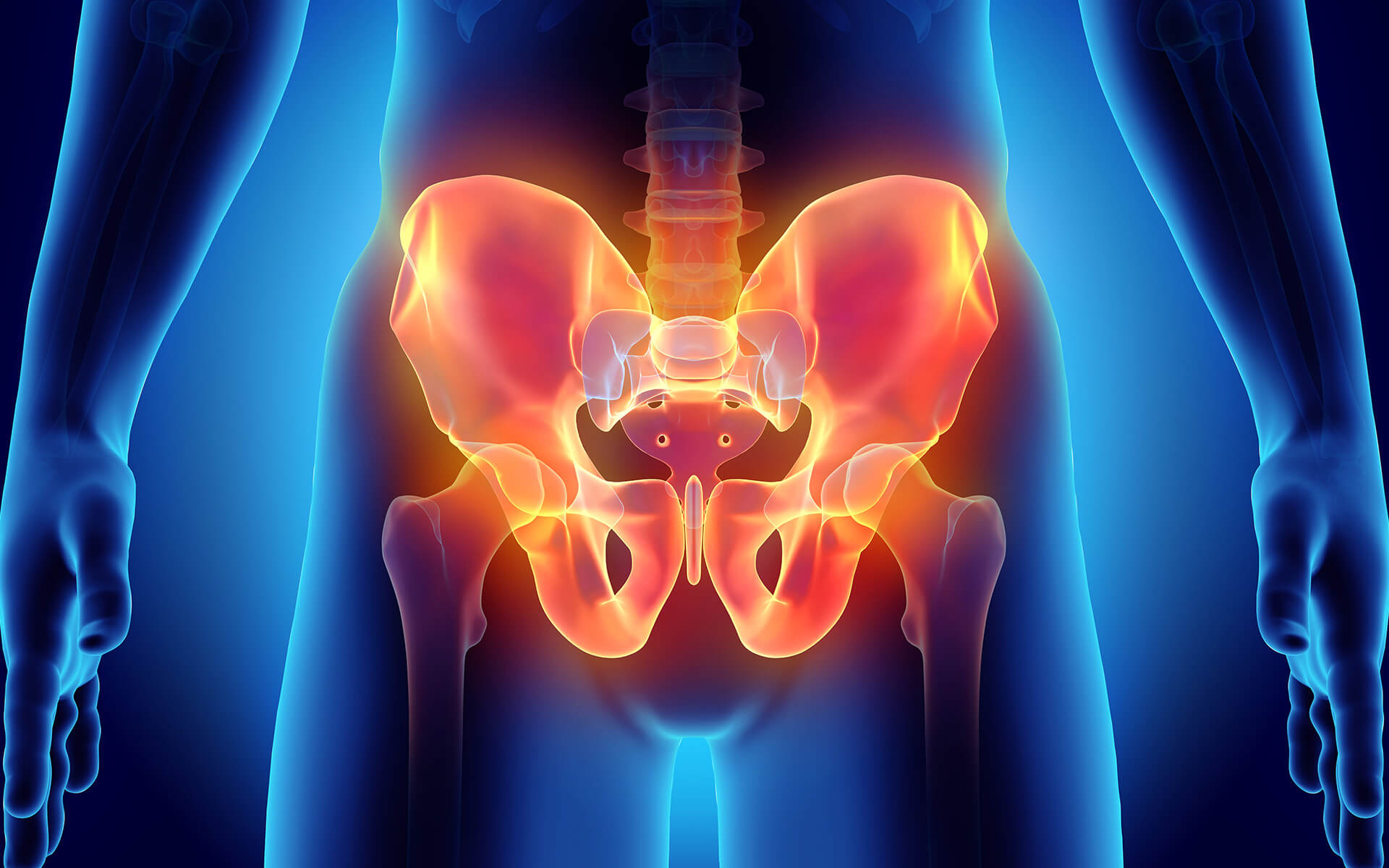
Pudendal neuralgia is a term meaning intense pain in the area in and around the pudendal nerve, which is located in the pelvic region. This intense pain is caused by the entrapment, compression, or dysfunction of the pudendal nerve.
Pudendal neuralgia, also known as pudendal nerve entrapment, cyclist’s syndrome, pudendal canal syndrome, or Alcock’s syndrome, is an uncommon condition which lasts for longer than 3 months and is often aggravated by the act of sitting down.
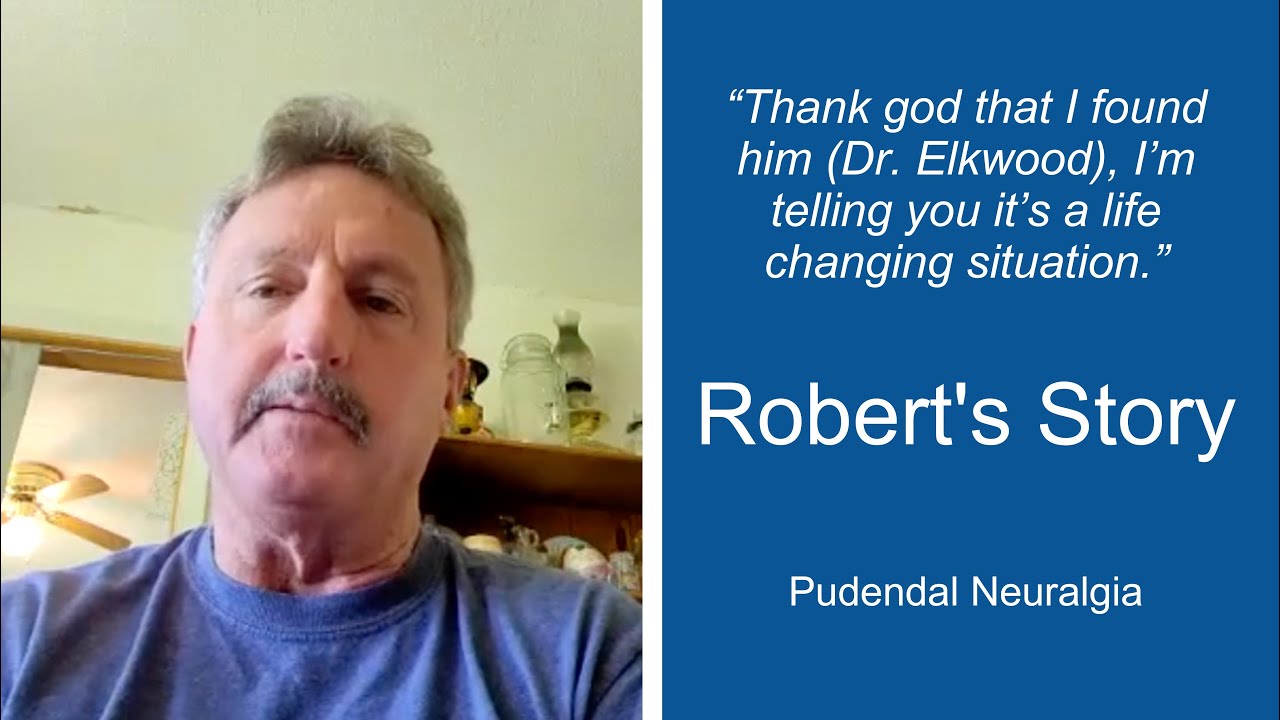
The Distinguished Center for Pudendal Neuralgia
Symptoms, Causes, and Treatment Options for Pudendal Neuralgia at The Institute for Advanced Reconstruction
Overview
Pudendal Neuralgia Symptoms
The primary symptoms of pudendal neuralgia include: burning, numbness, increased sensitivity, stabbing or aching pain, and abnormal temperature sensations. There are a variety of secondary symptoms which may indicate pudendal neuralgia as well. These secondary symptoms include:
- Sitting feels intolerable. Skin in the pelvic area may be hypersensitive to touch or pressure.
- Pain often not immediate but delayed and continuous during activity, and stays long after discontinuing the activity (e.g. standing, cycling, sex).
- Gradual increase in pain throughout the day.
- Loss of sexual sensation, difficulty achieving orgasm, or pain after orgasm – with or without scrotum/testicular pain.
- Feeling of uncomfortable arousal without sexual desire.
- Friction and feeling of inflammation when walking for too long or running.
- Constant pain even with standing or lying down.
- Feeling of a lump or foreign body in the vagina or rectum.
- Problem with urinary retention after urination, urethral burning with or after urination, or frequent urination.
- Constipation and pain with bowel movement.
- Lower back pain.
- Complex regional pain syndrome and even post-traumatic stress disorder after prolonged or severe pain.
Causes & Risk Factors
The potential risk factors and causes of pudendal neuralgia are fairly general. Luckily at the Institute for Advanced Reconstruction, we are as familiar with pudendal neuralgia as we are with the illnesses closely related to it.
Women and men are both capable of getting pudendal neuralgia, although around ⅔ of cases are women. Additionally, there are certain factors which are often the cause of pudendal neuralgia. These potential causes include:
- Cycling
- Childbirth
- Surgeries
- Squatting exercises
- Biomechanical abnormalities (e.g., sacroiliac joint dysfunction, pelvic floor dysfunction)
- Chronic constipation
- Repetitive vaginal infections
- Falls on the tailbone
- Sitting for long hours
- Other forms of physical trauma
Diagnosing Pudendal Neuralgia
Some tests can be used to help diagnose pudendal neuropathy; however, a large part of diagnosis also relies on a methodical study of the symptoms and personal medical history.
You will be asked your history, such as if you were exercising intensely, sitting long hours, or if you had been in an accident, vaginal delivery, or pelvic surgery. You will also be asked to pinpoint your pain, to determine if it is in the area innervated by the pudendal nerve.
In addition to a physical exam, testing may be used, such as electromyography to measure the electrical activity of muscle tissue surrounding the pudendal nerve and magnetic resonance neurography (MRN) to image the relevant nerves.
Image-guided pudendal nerve block, an injection with a local anesthetic performed by our experts, is the most important diagnostic test to determine if the condition is present. The final diagnosis of pudendal neuralgia is based on a person having several or all of these criteria:
- Typical PN symptoms
- An abnormal electrophysiological test (MRN, MRI)
- Pain elicited upon pressing along the anatomy of the nerve
- Elimination of other diseases or conditions as the cause
- A positive response to the pudendal nerve block
Pudendal Neuralgia Decompression Surgery
The Institute offers a specialized, minimally invasive procedure called pudendal nerve decompression. This procedure aims to carefully release compression points along the pudendal nerve pathway, relieving patients suffering from chronic pudendal nerve pain.
During the procedure, surgeons address areas where the nerve may be compressed or irritated by surrounding tissues, ligaments, or anatomical structures. By surgically decompressing these points of pressure, particularly in areas such as Alcock's canal or between the sacrotuberous and sacrospinous ligaments, pudendal neuralgia decompression helps restore normal nerve function and reduce the patient’s pain signals in that area.
After a pudendal neuralgia decompression surgery, patients typically stay in the hospital overnight, followed by 4-6 weeks of limited activity. Most patients can resume light daily activities within 3-4 weeks, gradually returning to normal activities over 8-12 weeks. Full recovery and continued improvement may extend up to six months.